August 2025 blog
There is now no difference between Labour and Tory! We need a pro NHS party in power
Labour promised
-"Change"-without defining what change...!
-"Privatisation on steroids..."
The purchaser:provider raised costs to 5-14%-£4.5to £10
billion a yerar
The HSCA pushed costs up to 30%
Germany-soaring admin costs 63% 1992-2003-20% of their health budget.
Every citizen paying in through tax is the most efficient! Tax should be linear
with earings!
“How to Dismantle the NHS in Ten
Easy Steps” Youseff El-Gingihy
the original work warning of their plans...
Step 6
Legislate for the Dismantling of the NHS
Nicholas Timmins “Never Again: The story of the Health and Care Act”- Lansley's Monster bill.
Tony Blair: Ram the bill through quickly-The public will have forgotten about it by the next election...
A smokescreen for free market reforms: The key words were "Any Qualified Provider"-private...
The NHS was being carved up into state insurance providers-like Medicare and Medicaid, with CGCs (Clinical Commissioning Groups) based on US managed care organisations acting as health insurers
Pollock, Price and Roderick:
- SoS no duty to provide
-devolved to CCGs-only to those on GP lists-EXCLUSION
-decide what services free
-rationing-budgets cut
Jeremy Hunt: the NHS should be privatised
The Act provides for atomisation and breakup
Consequencies of Lansley:
difficult to get new mental health units built.Provider groups have to send patients miles away to private units-
no PICU (psychiatric intensive care units) for children all of SW England
Highest risk mental units-greatest reliance on agency staff-agency worker-false identity-never worked at a hospital before-left patient alone. Understaffed
Another died-over fluid-nurses did not knowhow to use 999
Privatisation means profiteers taking salaries at every level, profits for shareholders as their prime duty: not best care...
Grassroots LibDems were against the Lansley Act, so was Shirley Williams-but fearing another election, caved in...
EveryDoctor: Alan Milburn, privatiser, is back...
He told the think tank that, “we’ve got to stop viewing the health care system in this country as being about a single institution that we happen to call the National Health Service, and instead see it as being an ecosystem of very different providers, from telecos, techcos, of course private sector providers, at the margins, the public sector, and that’s what it is”.
Years of ingnoring problems by government come home to roost...!!!
Events, dear boy... Recent and future events
Court cases...
BMA against GMC promotion of PAs... High Court case where the GMC (bribed with
£8 million) argued they were not responsible for patient safety (where
PAs, AAs are registered with them.) Permission given to appeal...
Anaethetists United against PAs-judgement awaited...
Leng review If you need time and space to recruit as many as possible-call
a review. The result is a hazy report which each side can quote to their cause.
10 year plan-meaningless without funding or delivery:TEN YEARS-need
ACTION TODAY!!!
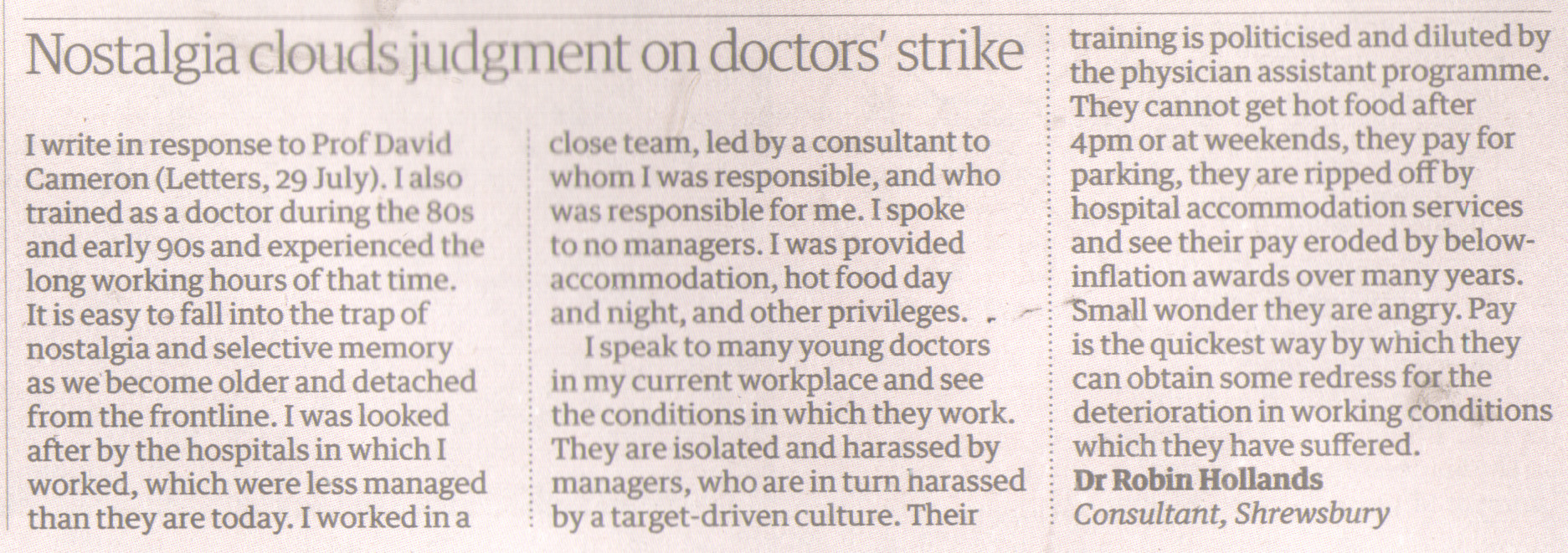
Workforce planning-lead by donkeys who could not plan a pissup in a brewery...
Every NHS and SC section requires more qualified staff. Government cuts mean
fewer staff, more leaving.Absolutely no succession planning for Consultants
of tomorrow!!!
Maternity, Doctors, Nurses, Midwives, beds
All the above are hampered by lack of funds-
proposals
1-can print money-Weimar-hyperinflation
2- Borrow more: IMF complains, cost interest increases
3-Could actually collect all taxes due! £46bn not collected last year!!!
Could tax oil, Google, Amazon correctly...
Tax the super wealthy...
Stop overseas tax havens...
Hippocratic oath
All medics (and Dentists!) swear on induction day (Why, o why, have I chosen
medicine/dentistry???)
First of all-do no harm!
Politicians never take the oath!
If I do not go into work-I caused no harm
I did go into work-I caused harm...
Politicians wage unholy war of words with the BDA and Doctors, GPs. Ancillary GPs staff require their pay uplifted.
Mackey: Multiple ACO providers to be created next year
ACOs are given a pot of money, allowed to keep after denying care...
https://go2.hsjinformation.co.uk/NTI1LVNIQS0zNTUAAAGbbzH-X3T2Rv0SXNgmu0O9HZMyOzOAeLhp143lk7FwGHW8V6tRZMEBjxS6g5RSJYqdG-moIjQ=
BDA NHS dentistry proposals:
Shiv PabaryGeneral Dental Practice Committee Chair
When I was elected GDPC Chair earlier this year, my first action was to reach out and listen to what you want to see from reform. We conducted a major survey to gather views on the sort of NHS dental service we would actually want to work in.
That consultation found a strong consensus on a wide range of points. Many of the ideas we put to you had greater than 95% agreement. It is extremely positive to see the profession speaking with a shared view and a single voice.
Agreement on the fundamentals
We’ve received strong support for a contract focused on prevention.
English GDPs want a contract that is practical, financially viable and simple; where payments reflect the costs of treatments; and patients know what is and isn’t available on the NHS. You told us that it was important that the NHS set a clear purpose for what dentistry is trying to achieve.
I’m incredibly grateful for this feedback. It will allow me and my negotiating team to go into our meetings with government with a clear understanding of what you want to see from a reformed contract.
The challenge for us now is to ensure that we open the door to the negotiating room and start those talks without any further delay.
Earlier this month, Stephen Kinnock MP became the first Dental Minister in decades to address a Local Dental Committee Conference. In itself, that sends a message, but it was also reassuring that his diagnosis of the state of NHS dentistry matched the reality we see in our practices. He acknowledged that the current situation is ‘Dickensian’ and the current contract is somewhere between a ‘treadmill’ and a ‘straitjacket’.
Speaking to LDC reps about contract reform, the Minister said, “While there is no one perfect payment system, we must build on experience, and we must address the contract in this parliament”. I agree with him on all three points.
"The challenge for us now is to ensure that we open the door to the negotiating room and start those talks without any further delay."
A blended contract
After nearly 20 years with the Units of Dental Activity (UDA) contract, I think all of us are crystal clear on what an imperfect payment system looks like. Contract reform must deliver a fundamental break with the UDA.
There is, of course, no single perfect alternative.
In developing our thinking and proposals for reform, we’ve focused on what will deliver a prevention-focused system, which works for different patients and different treatment types, and makes the NHS an attractive place to work.
That’s why the GDPC’s proposal to government has been for a contract that blends different types of payments so that the right funding and incentives are attached to the right types of patient care.
We think that weighted capitation is the best way to pay for routine care. We know that patients value a long-term relationship with their dentist, and that this is likely to help improve patients’ oral health. It also structures payments and care in a way that focuses on preventing oral disease, rather than just treating it once it develops.
Alongside this preventative routine care, there are still many patients who have high treatment needs. The UDA contract has failed them, and it is critical that a new system ensures they are cared for properly. We’ve proposed that there should be an activity payment for this treatment, probably based around an item of service model.
Then, there is urgent care, which comes with its own unique challenges. The time needed for each patient is unpredictable, as is demand for the slots and patients’ attendance. Sessional payments have been demonstrated to address these challenges and work successfully in Integrated Care Board commissioned schemes. This should be made the national model for urgent care.
There was a clear message from your survey responses that a reformed contract needs to be kept simple and practical. We will need to balance the desire for simplicity with ensuring that payments are a good fit for the clinical activity.
"A long-term relationship, focused on prevention, delivered results for improving individual patients’ oral health."
Learning from the prototypes
The Minister also said that we should learn from experience. He is absolutely right.
I worked at one of the around 100 practices that prototyped a different payment system based largely around capitation. At its heart was a clinical pathway that did dentistry the way we were taught at dental school. The model had many things going for it that could and should be brought over to a reformed contract. For me, the key thing was that a long-term relationship, focused on prevention, delivered results for improving individual patients’ oral health.
There are also things we can improve based on the learnings from that model. In the prototypes, the capitation payments weren’t weighted to reflect patients’ needs, meaning that those in high needs areas found it harder. There is a simple solution to this by applying weighting based on oral health need. The prototypes also used UDAs for some treatment, meaning patients with high needs continued to be under-funded. Again, the learning is clear: scrap the UDA.
Urgent progress
Now, we need to get down to the work of negotiating that contract. We are ready to start now, and the ball is firmly in the Government’s court.
We have made it clear to government that they have essentially run out of time. Dentists are already walking away from the NHS, reducing the number of UDAs they do, or packing it in altogether.
85% of survey respondents said that if we don’t see reform by the next election, they don’t think NHS dentistry will remain a viable service.
In the coming weeks, I expect NHS England will bring forward changes to the
UDA contract. We have discussed these proposals and fought for the very best
outcome for dentists and patients. These changes will, I hope, deal with some
of the worst aspects of the current system, but I am very clear that this is
not a substitute for real reform. The UDA is not fit for purpose and must be
scrapped altogether.
RCGP proposals for General Pactice GPs
Kamila Hawthorne MBE is Chair of Council for the Royal College of General Practitioners
and a GP in South Wales
As the Government prepares to unveil its 10-Year Health Plan (10YHP), the Royal
College of General Practitioners (RCGP) is calling for a bold vision and an
implementation strategy that prioritises improving patient outcomes through
a focus on prevention and community-based services.
General practice is the backbone of the NHS, providing essential care to millions of patients every year. However, the sector is facing unprecedented challenges, from workforce shortages (despite newly qualified GPs struggling to find jobs), to inadequate core funding and outdated infrastructure. We’ve seen a mere 150 increase in qualified GPs since 2019, despite the growing demand for services. This is the Government’s best opportunity to take game-changing action.
As Chair of the RCGP, I’m convinced that general practice is the linchpin of a sustainable, high quality and effective healthcare system. It is incredibly concerning to already see speculation that previous commitments to transfer funding to primary and community care might be delayed as part of the 10YHP, therefore we’re once again laying out why general practice must be prioritised if this plan is going to succeed on its aims.
The Government has already set out three key shifts for the plan to turn into reality: from hospital to community, analogue to digital, and sickness to prevention.
The Government has already set out three key shifts for the plan to turn into reality: from hospital to community, analogue to digital, and sickness to prevention. These are laudable goals, but we need to ensure that they’re backed up by a concrete implementation plan with action and investment.
From a primary care perspective, we believe that the measures of success should include improved GP access for patients, continuity of care, integrated care with streamlined patient records between all NHS services, and much more care delivered close to home. This will improve the patient experience of healthcare beyond measure.
Primary care at the heart of neighbourhood services
Without seeing the 10YP, we don’t fully know what is meant by a ‘neighbourhood health service’, but if properly designed with local communities, the concept has a lot of potential. To me, a ‘neighbourhood health service’ that works well would share care across health, social care, voluntary agencies and community services, such as community mental health services, palliative care and social prescribing. There would be specialised teams based in the community, which would look after more complex patients with long-term chronic physical and mental health illnesses, disabilities, and frailty.
GP teams are embedded in their local communities and know what their patients need. Primary care teams need to be properly resourced to take on a leading role in ensuring ‘neighbourhood health services’ are successful. GPs are skilled at leading multidisciplinary teams, treating and supporting patients with complex and multiple conditions, working closely with other community healthcare professionals and specialists where appropriate, as well as local authorities and the voluntary sector, and take pride in ensuring they can get to the root of what their patients really need. But these teams need the time, workforce, space and structural support to work effectively.
Preserving the universal ‘front door’ to the NHS
General practice needs to remain a universal ‘front door’ for patients, so that everyone can access a family GP to help them understand their health, manage a range of both acute and ongoing conditions, and stay well for longer. GPs need to continue to play a key role as ‘conductors of the orchestra’, helping to triage, refer patients to other services when needed, and navigate the healthcare system. GP practices would continue to operate in much the same way to the patients’ view (based on their patient registered lists), even if their back- office functions are being automated or shared across neighbourhoods.
Ensuring the GP voice
As ICBs go through another period of change, it’s crucial that frontline clinicians have a seat at the table when decisions are being made about how care is delivered. General practice staff need to be part of future planning at all levels of the new structures in the NHS, including those serving ‘neighbourhood health services’ (whatever they look like) and any frameworks over and above these. We must ensure that any new structures and commissioning systems for primary and community care are evaluated in real-time, to ensure they’re improving patient care, providing quality, cost-effective services, and identifying any unintended consequences.
Increasing the GP workforce
To deliver the ambitions set out for the 10YHP, we need a significant increase in the number of GPs. This requires building GP training capacity – both the physical space as well as the number of trainers (which are dwindling), creating long-term employment opportunities for newly qualified GPs, and supporting GP retention schemes. We also need to ensure that there are sufficient staff working right across the community, including in areas of deprivation. The forthcoming review of the NHS Long Term Workforce Plan must prioritise general practice and provide a roadmap for growth of key staff including GPs.
Investing in GP infrastructure
Our previous member survey found that 34% of GPs consider their premises unfit for purpose, and 84% said a lack of space limits their ability to take on GP trainees. We need at least £2 billion investment to fix practice buildings and make space for training and hosting new staff. Investment in primary care infrastructure would also facilitate co-location of community and voluntary services with practices, where this works for the local population and services.
Digitally enabling integrated patient care
A shared patient record is crucial for truly integrated working across the NHS and beyond. Patients should be more involved in deciding how they receive care, through an enhanced NHS App that would allow them access to their own records and test results, and the ability to book their appointments. We’ve seen attempts to progress this in the past, but progress has been painfully slow due to the size of the challenge. Dedicated funding, time, and energy are needed to make sure patient record systems work effectively, securely, and safely for staff and patients. Patients should be able to choose the care they need and access information about their care at their fingertips.
Focusing on prevention
With the right resources and enough time with patients, general practice can
do much more in both preventing sickness and illnesses getting worse.
GPs understand the health of their local patient populations and the opportunities
that could help improve their health. With the right resources and enough time
with patients, general practice can do much more in both preventing sickness
and illnesses getting worse. To enable a real shift towards prevention, there
needs to be a further shift away from targets for NHS activity towards measuring
improved local population health outcomes.
Moving more funding into the community
To ‘shift care from hospitals into the community,’ and to achieve what I’ve set out above, a significant uplift in primary care funding is essential. We’ve seen years of underfunding of general practice, which has resulted in a lack of resources and capacity. RCGP is calling for a Primary Care Investment Standard, ensuring that both central government and Integrated Care Boards (ICBs) increase their spending on general practice and primary care each year.
Conclusion
The 10YHP presents a vital and exciting opportunity for the Government to transform the NHS and put patients first. By focusing on general practice, investing in GP workforce and infrastructure, and encouraging an emphasis on prevention, we can deliver a healthcare system that genuinely is fit for the future. The RCGP is committed to working with the Government and other stakeholders to make this vision a reality. Let’s put patients at the heart of the NHS and build a healthcare system that truly serves their needs.
Deputy Editor’s note: This paper summarises the RCGP’s key recommendations to Government and regional decision-makers as they refine details about how the plan will be implemented over the coming months and years. The RCGP’s full detailed response to the Government’s consultation on the Plan in December 2024 can be found here.
Featured photo by Nicholas J Leclercq on Unsplash.
https://go2.hsjinformation.co.uk/NTI1LVNIQS0zNTUAAAGcKIfTo7ASs8ZXwhehcQgoQNM6eTayHBrqr9ITNBXovNRiEC_5X6yxYu4v6qrM9XYmLknfsn0=